Last updated on January 31st, 2022
Diabetes occurs when the immune system accidentally attacks and destroys insulin-producing cells in the pancreas. Insulin is a body hormone that is necessary for metabolism as it processes carbohydrates from food. Without sufficient insulin, blood sugar levels can skyrocket or fall short, leading to severe complications or death. People with DM type 1 have to replace lost insulin using insulin injections or an insulin pump. Read this article to know about the relationship between dysfunction of thyroid and diabetes mellitus
Diabetes is a disease that causes the most deaths worldwide. It causes alterations in glucose metabolism derived from the low availability of insulin or resistance to its action. Recent studies and research indicate a relationship between dysfunction of thyroid and diabetes mellitus, mediated by disturbances in the hypothalamic-pituitary-thyroid axis. It reduced deiodinase activity, synergism of mutagenic pathways, increased inflammatory status, oxidative stress, and insulin resistance. The most frequent alteration is subclinical hypothyroidism, and it occurs more frequently in females, so it is suggested to perform a thyroid profile in these patients periodically.

Type 1 Diabetes and Thyroid
Most of the time, people with DM type 1 develop hypothyroidism, a condition known as Hashimoto’s disease. About 10 percent of the time, type 1 diabetes and thyroid are closely related.
Untreated or poorly treated thyroid problems can affect blood sugar levels in people with type 1 diabetes. Knowledge of both diseases can help in the excellent management of both type 1 diabetes and thyroid. Sometimes people with DM type 1 gain weight when taking insulin, but unexplained weight gain can also be due to an underactive thyroid.
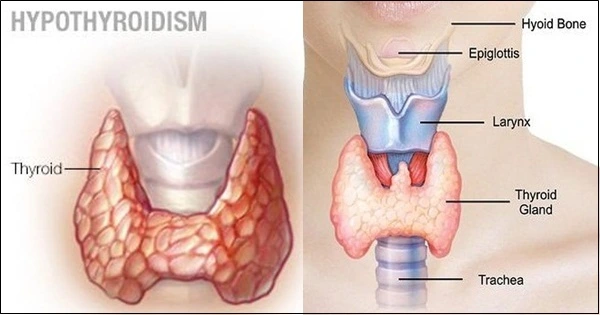
The classic symptoms of hypothyroidism are decreased energy, hair loss, inappropriate weight gain, feeling cold, constipation, dry skin, heavy periods, and difficulty concentrating. Some of the symptoms also overlap with the diagnosis of depression. Thyroid dysfunction (TD) in adults, understood as hypo and hyperthyroidism, has a systemic impact on all tissues of the economy through the action of the hormones thyroxin (T4) and triiodothyronine (T3).
Its clinical presentation is adaptable, and in the case of hypothyroidism, its installation is usually chronic and insidious. It can go unnoticed or be confused with manifestations attributed to other conditions, leading to diagnostic delay and timely treatment. The diagnosis and treatment of these conditions are accessible and, particularly for hypothyroidism, a meager cost. Proper treatment normalizes thyroid function and avoids major complications in both circumstances, among which cardiovascular repercussions stand out.
Likewise, it improves patients’ quality of life, and complying with secondary prevention for severe complications with minimal cost avoids unnecessary expenses for the health system. Therefore, it is understood that it is of interest to have information about its frequency in each country or region.
Also Read: Diabetes and Heart Disease

Emergence of TD in a Diabetic State
Summary
The prevalence of TD varies in different geographical areas, is related to race, iodine intake, and, like other endocrinopathies, increases with age, with hypothyroidism being much more frequent than hyperthyroidism. Already the Whickham study in 1977 warned about its frequency in adults and fundamentally in those over 45 years of age. The more specific and early clinical diagnosis of functional alterations and new laboratory techniques for hormonal determinations are factors for this increase, not finding references to other parameters that may influence.
The emergence of thyroid and diabetes symptoms is subject to crucial modifications that occur in different processes. It is easy to think about the possibility of finding a close relationship between DM2 and TD if it is taken as a basis that insulin and thyroid hormones are responsible for regulating metabolism.
In principle, we speak of changes in the hypothalamic-pituitary-thyroid neuroendocrine axis. These changes appear to be caused by IR and subsequent compensatory hyperinsulinemia. Thanks to the anabolic effect of insulin, there is an improvement in the availability of TSH. The serum concentration of peptide C is released together with insulin from the β cells in the pancreas from the proinsulin.
Until recently, it was believed that this peptide was non-functional, but today it is known that it modulates some cellular functions by binding to a surface receptor coupled to protein G. One of its effects is to favor the activity of the sodium-potassium ATPase (Na + -K + ATPase) necessary for the protein synthesis of many hormones including THS.
However, more studies are required to elucidate the pathophysiology of this process, since studies in animals show that during induced diabetes, there is a reduction in the synthesis and therefore in the serum levels of thyrotropin-releasing hormone (TRH) produced from the hypothalamus, which simultaneously leads to a decrease in serum TSH, T4 and T3.
Disorders in the conversion stage of T4 to T3 have also been evidenced in some target cells such as hepatocytes in response to decreased expression and function of deiodinase enzymes, making it possible to find low levels of T3 12. Even supports indicate that during prediabetes, low levels of free T3 (FT3) are accompanied by an atypical increase in reverse T3 (rT3), an alternate product of T4 dehalogenation with less biological activity than T3.
Autoimmune and inflammatory factors are another aspect to consider. Patients with DM1 are more likely to develop autoantibodies directed against other endocrine glands in addition to the pancreas, including the thyroid. Anti-thyroglobulin (Tg-Ab), anti-thyroid peroxidase (TPO-Ab), anti-TSH receptor (TR-Ab), among others, can be found in these individuals. Now theories have been put forward that defend that the emergence of TD in DM2 is due to autoimmune causes.
The chronic inflammatory state of DM2 is related to the elevation of cytokines such as tumor necrosis factor-alpha (TNF-α), interleukins 6, 8, and 1 (IL-6, IL-8, IL-1), and leptin, coming mainly from macrophages in adipose tissue and oxidative stress possibly produced by the elevation of metabolites such as carbohydrates, lipids, and fatty acids. Thus, obesity should be considered a factor synergistically involved in developing complications associated with 18, and 19.
Recent research reveals the existence of a direct correlation between IR, obesity, and adipocytokines with dysfunction of the sodium-iodide symporter (NIS). This membrane protein facilitates active iodide transport in follicular cells and enterocytes, translating into low serum levels of the anion and alterations in thyronine synthesis 20.
The increase in oxidative stress due to the acceleration of the respiratory chain facilitates the appearance of reactive oxygen species (ROS), the increase in nitric oxide (NO), and the consumption of endogenous antioxidants. Furthermore, the permanent exposure of glucose to serum and constitutive proteins favors their interaction and subsequent irreversible binding through glycation mechanisms, forming different advanced glycation end products (AGEs). These imbalances have been implicated in the pathogenesis of thyroid autoimmune diseases 21, 22, 23.
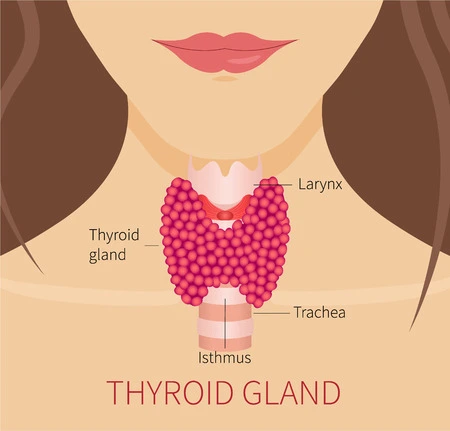
Finally, the superposition of mitogenic pathways mediated by high levels of insulin, insulin-like growth factors 1 and 2 (IGF 1 and 2), epidermal growth factor (EGF), and glucagon-like peptide -1 (GLP- 1) act as growth factors of the cells that make up the thyroid, which alters cell division and epithelial morphology. Supporting the above, some studies indicate that the prevalence of thyroid nodules increases with the simultaneous presence of DM, in part due to the overexpression of IGF in follicular cells and C cells; even more serious, this growth stimulus is one of the agents considered as triggers of thyroid carcinoma (TC). In most of these malignant cells, insulin receptors and IGFs are over-expressed 9, 24, 25.
Also Read: Age 50 70 Sugar Level Chart Age Wise
Complications Due to Thyroid Dysfunction During Type-2 Diabetes
Summary
The TD with the highest prevalence in populations with DM2 is hypothyroidism, specifically subclinical hypothyroidism, although hyperthyroidism is also evidenced to a lesser extent. This condition establishes a significant relationship with age and has a substantial predominance in the female sex. The appearance of the type of DT is subject to certain conditions such as the population group studied, ethnicity, and environmental factors 5, 26, 27.
There is greater metabolic involvement, especially concerning the movement, transformation, and use of glucose, lipids, and amino acids, which predispose to the appearance of cardiovascular diseases such as atherosclerosis, coronary heart disease, vascular accidents, and hypertension 28. There is an increased risk in the development of nephropathy, neuropathy, diabetic retinopathy 29, 30.
This hurts the morbidity and mortality rates of subjects with DM2. It should be considered that both DM2, hypothyroidism, and arterial hypertension are diseases that appear silently and that can remain hidden for long periods, hence the need to promptly intervene in the diabetic patient to prevent complications and improve their expectation life 31.
Hypothyroidism
Summary
In general, in diabetic hypothyroidism, there is a slow consumption of insulin, low glucose availability, delayed gluconeogenesis, and increased total cholesterol levels, which can easily lead to hypoglycemia and predisposing to the appearance of acute coronary syndrome. Meanwhile, in hypothyroidism and diabetes, there is more excellent intestinal glucose absorption and more significant generation by gluconeogenesis, which makes it challenging to control glycemia by increasing IR 3.
Within the clinical practice, the diabetic patient should be treated with care, bearing in mind that DM type 2 is a risk factor for the appearance of thyroid dysfunctions, which include not only the thyroid gland and the hormones produced there but also the hypothalamic axis – pituitary and deiodinase enzyme activity in target tissues. These alterations are primarily caused by insulin resistance, hyperglycemia, oxidative stress, the joint activation of mitogenic pathways, and obesity seen from the mediating role in chronic inflammation.
A systematic analysis of the thyroid profile could favor the control of glycemia and lipemia by facilitating timely diagnosis and treatment, preventing other complications such as derived cardiovascular diseases, and reducing morbidity and mortality.
Conclusion
The thyroid diabetes have a complicated interdependent relationship. In patients with Graves’ illness, insulin resistance may enhance thyroid gland nodularity, and accompanying diabetes may increase the chance of vision loss. In hyperthyroidism and diabetes affects glycemic control, whereas hypothyroidism increases hypoglycemia susceptibility, complicating diabetes care. Thyroid hormones may also influence glucose metabolism through leptin, adiponectin, and gut hormones like ghrelin. However, more investigation into this link and the consequent changes in metabolic processes is required. The diabetes thyroid problems are more prevalent in patients with diabetes, particularly type 1 diabetes.
Furthermore, undiagnosed thyroid dysfunction appears to harm diabetes and its consequences. Diabetic patients with subclinical hypothyroidism had a higher prevalence of retinopathy and nephropathy and more severe retinopathy. As a result, treating subclinical hypothyroidism in diabetic individuals may be advantageous as there is a link between hypothyroidism and diabetes. It is concluded that a systematic approach to thyroid testing in diabetes patients is beneficial. However, there are no established standards for thyroid dysfunction screening in diabetes individuals. Finally, whether all diabetic patients should be evaluated for thyroid function or whether individuals with subclinical thyroid illness should be treated is debatable.
Also Read: Diabetes and Sleep Apnea
FAQs:
Can your overactive thyroid be related to diabetes?
Based on a study it was revealed that overactive thyroid and diabetes often exist simultaneously in patients. Considering both are associated with the dysfunction of endochrine glands in the body.
Can diabetes cause hyperthyroidism?
Yes, it is possible diabetic patients are more at risk of developing thyroid disorder.
Does thyroid affect blood sugar level in the body?
Considering that thyroid hormone is responsible for balancing several body processes, such as metabolism. Due to which it can have an impact on the blood sugar level as well. Both hyper and hypo-thyroidism are associated with increased blood sugar level. Thus, it is common that thyroid condition can affect the blood sugar level.
What is the best way to find out if I am hypothyroid?
Diagnosis of hypothyroidism requires documentation of low levels of thyroid hormones (i.e., T4 and T3). However, the diagnosis is refined by measuring thyroid-stimulating hormone (TSH) produced in the brain and acts on the thyroid gland to stimulate T4 and T3 production. If TSH is high, then thyroid gland hormone secretion is the primary defect. However, if TSH is low, then the inadequate supply of this hormone from the brain (pituitary gland) is the cause of hypothyroidism.
Does hypothyroidism cause diabetes?
Type 1 diabetes, type 2 diabetes, and gestational diabetes are caused by a deficiency of insulin in the body’s ability to digest sugars and carbohydrates. Hypothyroidism causes a decrease in insulin sensitivity, which raises blood sugar levels as a result we also have a answer to the question can hypothyroidism cause blood sugar issues. Obesity, a leading cause of diabetes, is also caused by a high body mass index.
References:
- https://www.verywellhealth.com/thyroid-disease-and-diabetes-3289616
- https://www.hindawi.com/journals/jtr/2011/439463/
- https://www.diabetes.co.uk/conditions/thyroid-disease.html
- https://www.verywellhealth.com/thyroid-disease-and-diabetes-3289616
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3139205/
Last Updated on by Dr. Damanjit Duggal
Disclaimer
This site provides educational content; however, it is not a substitute for professional medical guidance. Readers should consult their healthcare professional for personalised guidance. We work hard to provide accurate and helpful information. Your well-being is important to us, and we value your feedback. To learn more, visit our editorial policy page for details on our content guidelines and the content creation process.

 English
English